Mark is lying on the operating table right in front of me, and it is obvious that his day has taken a turn for the worse. Which is too bad, because his day started out quite well.
About three hours ago, this 42-year-old scientist and seasoned long-distance runner went into surgery to remove a malignant thyroid tumour. Following an uneventful procedure, the surgeon closed up the wound, and now the tumour is sitting peacefully on a table not a metre away from me. Aside from the fact that he’s short one thyroid gland, Mark was otherwise hunky dory.
Now, however, Mark is not doing well. In fact, he’s rather sick. Actually, truth be told, he’s dead.
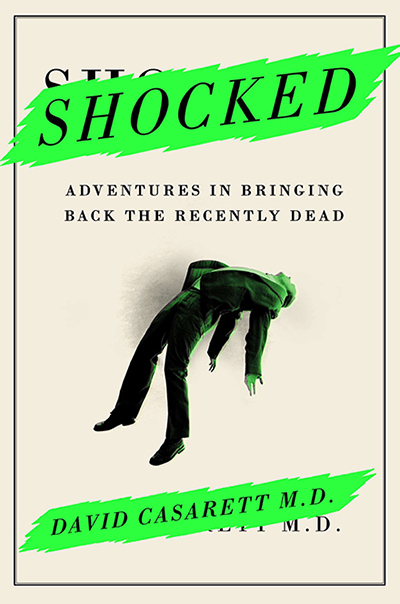
This is an excerpt from SHOCKED: Adventures in Bringing Back the Recently Dead, by David Casarett, MD, reprinted with permission of the Penguin Group (USA).
I know this because Mark is not moving, breathing, or performing any one of a number of behaviours that are usually reliable signs of life. I also know this because there’s a monitor to my right that displays all of his vital signs, which are pretty conclusively absent. For instance, I’m watching his respirations (nil), heart rate (zero), blood pressure (zip) and EKG tracing (flat). It’s a textbook case of someone who is undeniably and incontrovertibly late.
And yet, despite the tragically premature death of this 42-year-old man, the eight doctors and nurses gathered around the operating room table are giggling nervously. An anesthesiologist is trying mightily to force air into Mark’s lungs, but those lungs do not seem to be cooperating. A surgeon is poking at Mark’s neck with a scalpel in much the same way that you might poke a beehive with a stick. Which is to say, without any demonstrable enthusiasm whatsoever.
Unless something miraculous happens, it’s looking increasingly likely that our weekend athlete will never run another marathon. Still, the giggling continues. This, I’m thinking, is going to be difficult to explain to Mark’s bereaved family.
Fortunately, though, that conversation won’t be necessary. This isn’t a real operating room, and Mark isn’t a real patient. I’m actually in the University of Pennsylvania’s simulation center that is designed to recreate the circumstances, confusion, and anxiety of real medical emergencies. All of this — the EKG tracings, the history, and even the trappings of the operating room around us — are the set and props of an elaborate drama that helps OR teams learn to respond to the unexpected.
At the heart of this simulation is our patient, known today as ‘Mark.’ He’s actually a metal and plastic mannequin. His history is fabricated and his physiology is simulated.
However, he’s designed with careful attention to detail, so that the team of doctors and nurses surrounding him can do virtually anything they would to a real patient. For instance, when the anesthesiologist inserts a breathing tube into Mark’s lungs, a sensor displays the resulting increase in oxygen on a monitor over the operating table. It’s a truly amazing arrangement that tells the team what they’re doing well. Or not, in Mark’s case.
Suddenly, though, Mark’s future is looking just a little brighter. A nurse has wheeled in an automatic defibrillator — a plastic box the size of a milk crate. It’s equipped with handy wires that the team attaches to pads on Mark’s chest. The room is quiet for a moment, and then the defibrillator springs to life.
We all breathe a sigh of relief. It’s like everyone’s favourite extrovert has just made a grand entrance at a hopelessly dull party. But it only takes about two seconds for me to wish that this particular guest hadn’t been invited.
As soon as it’s powered up, the new arrival demonstrates that it has the capacity for speech. (This isn’t unusual. Most defibrillators, and particularly those that are used in public settings, provide audible information about the rhythm that they detect, as well as instructions for bystanders.)
Unfortunately for all of us, this particular defibrillator has a harsh electronic voice that somehow manages to be both abrasive and dripping with ennui. In short, it reminds more than a little of the evil Daleks of Dr. Who fame. And it’s using that voice right now to tell the team to “continue CPR.”
The Dalek’s advice is greeted with more than a little eye-rolling by the doctors and nurses who have doing exactly that, for the past five minutes. They know that Mark has no detectible heart rhythm. That is, he’s in asystole, so there’s no abnormal rhythm to shock. I’m afraid that this machine hasn’t lived up to the expectations its theatrical entrance generated.
But suddenly, much to everyone’s surprise, now Mark’s heart has a rhythm. It’s an abnormal rhythm, but it’s a rhythm. And that’s good news. The Dalek can’t contain his enthusiasm. After a moment’s analysis, he renders a diagnosis.
“Ventricular fibrillation” he announces proudly. “Stand clear,” he warns. If this Dalek defibrillator were a real person, he would be puffing out his chest and strutting with self-importance. Now he’s the center of attention. He’s the man.
The defibrillator administers a shock, and then the doctors and nurses descend like birds diving onto a pile of breadcrumbs. But Mark is still in ventricular fibrillation, and again, there’s no pulse. So they follow a carefully choreographed protocol of CPR and intravenous drugs, with brief pauses for the defibrillator to administer more shocks.
After a few minutes, one of the nurses notices that Mark’s heart has a normal rhythm. He’s alive. There are high fives all around as the team heads off to debrief. But the poor defibrillator that saved the day lacks arms or hands, and is left out of the victory circle. Almost as an afterthought, one of the last nurses out the door reaches over and flicks his power switch as she passes. I swear I can hear a despondent sigh as his lights flicker and then go out.
David Casarett, MD, is a physician, researcher and tenured professor at theUniversity of Pennsylvania Perelman School of Medicine. His studies have included more than 10,000 patients and have resulted in more than one hundred articles and book chapters, published in leading medical journals such asthe Journal of the American Medical Association and The New England Journal of Medicine. His many awards include the prestigious US Presidential Early Career Award for Scientists and Engineers.
Reprinted from SHOCKED: Adventures in Bringing Back the Recently Dead by David Casarett with permission of Current, a member of Penguin Group (USA) LLC, A Penguin Random House Company. Copyright (c) David Casarett, 2014.
Picture: Shutterstock / sfam_photo
