A widely used and cheap steroid treatment appears to be the first to show a definitive lifesaving benefit for people with severe covid-19. In a large clinical trial funded by the UK government and others, the drug dexamethasone was found to reduce the odds of death in patients who needed a ventilator to breathe by a third, compared to standard supportive treatment; it also seemed to help save people sick enough to need supplemental oxygen.
The preliminary results came from the UK’s RECOVERY study, one of the world’s largest randomised and controlled clinical trials intended to test out a number of potential treatments for covid-19. Earlier in the month, data from RECOVERY found that the antimalarial drug hydroxychloroquine had no benefit on reducing deaths, which seemed to influence the U.S. Food and Drug Administration’s decision this week to pull an emergency use authorization for the drug as a covid-19 treatment.
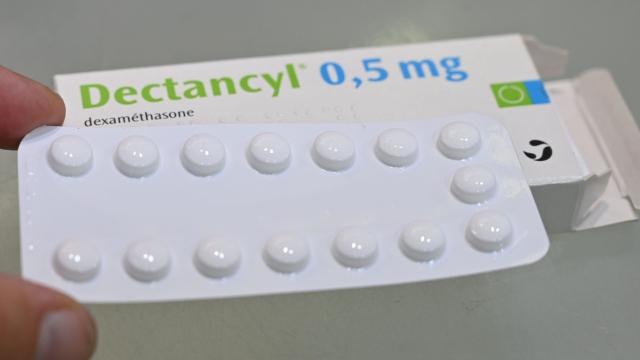
On Tuesday, researchers from the University of Oxford released the results from another arm of the trial, testing out the drug dexamethasone. Like steroids in general, dexamethasone tamps down harmful inflammation and suppresses an overactive immune system. Since the 1960s, it’s been used to treat a variety of conditions, including arthritis, autoimmune disorders, and many breathing disorders.
From very early on in the pandemic, doctors had suspected that steroids could prove helpful for severe cases of covid-19, which is often characterised by widespread inflammation that damages the body and can limit someone’s ability to breathe. But there hasn’t been definitive evidence to date, as well as some concern that these drugs could even worsen outcomes.
According to Oxford researchers, the trial involved over 2,000 patients who were given dexamethasone. These included people in very critical condition on ventilators as well as those with less severe illness who were given oxygen feeds.
Compared to standard treatment, dexamethasone seemed to reduce the chances of dying by a third for ventilator patients and by a fifth for patients on oxygen. There was no added benefit to survival for severe cases that didn’t require either a ventilator or oxygen. Given the results, the researchers estimate that the drug would prevent one death per every eight patients on a ventilator and one death per every 25 patients on oxygen who was treated with it.
While other trials or observational studies have suggested that some drugs may shorten the course of illness or reduce symptoms, this is the first trial of its kind to clearly show a lifesaving potential from a treatment. It’s understandably left the researchers excited.
“This is an extremely welcome result,” said study author Peter Horby, an emerging infectious diseases specialist at Oxford, in a statement released by the university. “The survival benefit is clear and large in those patients who are sick enough to require oxygen treatment, so dexamethasone should now become standard of care in these patients. Dexamethasone is inexpensive, on the shelf, and can be used immediately to save lives worldwide.”
A very important caveat here is that the data from this trial has not been peer-reviewed and independently verified by other researchers. There needs to be other research that supports these findings in order for dexamethasone to become a gold standard of treatment moving forward. But in a pandemic that has offered few morsels of hope, especially when it comes to useful treatments, this is undoubtedly good news.