STIs in the United States have been on the rise in recent years, and many marginalised people who are most at risk aren’t getting tested and treated for them. But remote healthcare is also on the rise—we are moving toward a future where at-home sexual health screening services could ease access to diagnosis and treatment for patients who aren’t getting the care they need.
With Planned Parenthood currently facing a funding crisis and many rural areas simply not able to serve their populations with appropriate sexual health care, there are folks all over the country who are isolated and denied care. But it’s not just physical access that prevents patients from getting screened for STIs.
Trauma can also play a role in a person’s choice to get screened. Sexual assault survivors are more likely to avoid STI screenings—and not just in the cases of forensic examinations and follow-up visits. A UK study found that women who had been sexually abused were less likely to get cervical screenings, including Pap smears to detect human papilloma virus (HPV), the STI that can cause cervical cancer. Pap smears are more invasive than other STI tests; to perform a Pap smear, healthcare professionals must insert a speculum into the vagina and then brush away cells to be tested for abnormalities. It’s no wonder that patients with a history of trauma may be hesitant to undergo these procedures, when a 2018 survey found that some young women don’t get tested because they are not comfortable simply discussing sex and STIs with their doctors.
Additionally, transgender patients are more likely to avoid STI testing, even though they face a high risk of STIs. This is a symptom of a larger issue with the healthcare system, as trans people continue to report being systematically disrespected and misunderstood by their healthcare providers.
Until the U.S. medical system reforms to treat trans patients, survivors of sexual violence and other marginalised groups with specialised, professional and respectful care, healthcare will continue to be unequal for these groups. However, tools that allow patients to perform tests on themselves in the comfort of their homes could get rid of some of the inconvenience, embarrassment, and other issues that sometimes prevent people from getting tested.
The more people are able to diagnose and treat STIs, the easier it will be to contain their spread. However, as the number of remotely available healthcare services continues to grow, it’s important that patients don’t try to use them to replace ongoing relationships with their doctors.
Nurx, a company that started out providing patients with remote birth control access, started selling at-home STI kits in the U.S. in July. According to Allison Hoffman, Nurx’s brand and communications lead, “There are people who unfortunately have had… negative or even traumatic experiences in the healthcare system. We’ve certainly heard that from our patients as well,” adding that at-home testing gives patients “a platform where you’re not necessarily facing the power dynamic of like sitting there with a doctor in a white coat and stethoscope.” Nurx offers a variety of at-home STI testing kits—some of which screen for STIs in the throat and rectum as well as in the blood and genitals, a rarity in most clinics. The home screening options include tests for chlamydia, gonorrhea, syphilis, trichomoniasis, hepatitis C, and HIV. (Herpes screenings are not offered.)
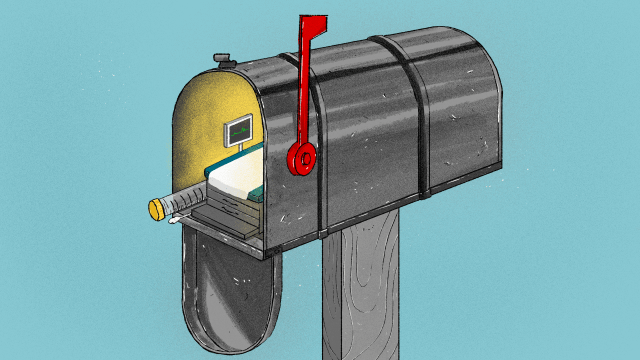
These kits include swabs to collect cell samples and needles that allow patients to provide small blood samples, similar to insulin tests for diabetic patients. After collecting their samples, the patients send them back to the company in a prepaid envelope and then receive results in five to seven days, according to Hoffman. If a patient tests positive for an STI, the company provides remote antibiotic prescription service or helps patients find the in-person treatment they require.
The kits cost between $US150 ($219) and $US200 ($292) for patients without insurance and $US75 ($109) for those who do have insurance and are available to Medicaid patients in California, Texas, and Illinois. In-clinic testing is often cheaper than this, so these prices are potentially prohibitive. Many insurance plans cover STI testing without cost sharing. And for uninsured patients, more cost-effective options are often available at places like Planned Parenthood and free clinics. However, in more rural parts of the U.S., facilities like those could be hours away, and Planned Parenthood’s funding crisis puts existing access into jeopardy.
Hoffman claims that in the first month that Nurx began offering at-home STI testing, the company found that its customers were more likely to test positive for STIs than patients who go to clinics in person, suggesting that the services might be reaching patients who have not been screened in the past, said Hoffman.
But there are concerns with at-home screening, especially since these services are still very new. One downside is the potential for patient error.
Hoffman said that at Nurx, they’ve found “overcommunication is key,” to make sure patients correctly follow instructions when taking at-home STI tests. She said the company learned from its experience providing at-home HPV screening, which it piloted six months ago. “That’s given us a really good signal in terms of thinking… we should add an extra sentence here to make sure this part is really explicit.” Studies of both men and women self-collecting cell samples from their genitals do suggest that various self-collection methods, when done correctly, are comparably sensitive and accurate to in-clinic collection.
Nathaniel DeNicola, chair of telehealth at the American College of Obstetricians and Gynecologists, said at-home screening services are likely to reach people who are more comfortable doing a test on themselves than they are getting an intimate examination from a doctor.
DeNicola adds that by including follow-up care as part of the package, at-home screening services could help ensure that patients actually learn their results and get the treatment they need. Clinics that provide STI testing aren’t always able to get patients to come back for follow-up care.
When speaking broadly about follow-up care by at-home STI screening services, founding medical director of UCSF Transgender Care Madeline Deutsch stressed that the appropriate way of disclosing test results from an at-home screening service would by professionals trained as STI and HIV counselors. While there are several companies already offering at-home testing, these types of companies generally offer referral services, not direct counseling, as in the case of OraQuick, an at-home HIV testing provider.
“I do think that we’re at a point in society where we have to look at this direct-to-consumer telehealth testing market very carefully,” Deutsch said, referring to the way in which test results are disseminated to the patients. She also stressed the importance of follow-up, in-person counselling, such as detailed discussions of appropriate treatment and family planning.
“It is a very fine line between the positive benefits of this type of service and the negative,” she continued. “The big question is, is there a trained counselor who can talk somebody through the results on the other end of these phone lines? And also, are those specific to transgender care? Are those people specifically trained on transgender health issues and do they have resources they can tap into to connect, to link a person to care if they are transgender and have tested positive for something to link them to a trans-appropriate resource?”
Nurx’s Hoffman insisted that the company’s clients have “unlimited access” to a Nurx provider, and specifically, while “We do not have any particular services for transgender patients or patients who have experienced sexual trauma… our medical team also has extensive experience working with these types of patients.”
In speaking to way the sensitive test results are disclosed, Hoffman described that “all HIV results are disclosed to the patient in a sensitive and knowledgeable fashion, following state laws around result disclosure. Our team of medical providers and nurses are equipped with HIV education and links to care resources for confirmatory testing and ongoing HIV treatment. We work closely with each patient to help them get in-person care, and we stay connected with them until we know they are well established with their new HIV treatment provider.” The counseling offered by Nurx also “can certainly include recommendations on how to speak with their partner(s) about their HIV status.”
With telehealth practice on the rise, sexual health self-screenings could eventually become a standard component of an expanded medical system. The prospects of reaching marginalised groups of people is highly encouraging, as long as the services follow best practices, such as providing dependable follow-up assistance and resources to in-person care to patients.
As a whole, the current U.S. medical system requires substantial reform to properly serve at-risk communities and to properly serve everyone. This future could include a convenient, affordable telehealth component such as at-home sexual health screenings.
Hannah Harris Green is an independent writer and audio producer interested in the intersections of gender, sexuality, health, and tech.