It’s still flu season, but a preliminary report by the US Centres for Disease Control suggests this year’s flu shot is nearly 50 per cent effective at reducing a person’s chance of getting sick. This is actually pretty good considering that, just two years ago, the flu shot’s effectiveness was down at a paltry 19 per cent. Here’s why the flu shot varies so widely from year to year — and why you should get a shot this year if you haven’t already.
The CDC doesn’t know the exact rate at which the flu vaccine confers immunity in a given year, but by counting the number of vaccinated people who come in for a doctors visit, it can approximate the performance of the shot. For the 2016-2017 flu season, the CDC estimates the effectiveness of the influenza vaccine at 48 per cent, meaning that’s how much a person’s risk of getting sick and having to seek medical attention is reduced.
That’s significant. The CDC says it’s not too late to get the flu shot, especially when the virus is still circulating — which it is. The length of the flu season varies each year, sometimes pushing into late May.
The interim report, compiled by the CDC’s Flu Vaccine Effectiveness Network, suggests the flu shot’s effectiveness is around 43 per cent for the predominant influenza A viruses (the strains known as H1N1 and H3N2), while the effectiveness against influenza B viruses (B/Yamagata and B/Victoria) are as high as 73 per cent. This makes sense, given that influenza B drifts, or mutates, at a rate two to three times slower than influenza A. Influenza B tends to cause a less severe reaction than type A flu virus, and is not capable of causing pandemics.
The reason for influenza’s success, and why a new flu shot is required each year, has to do with that rapid mutation rate. Unlike some DNA-based viruses, influenza uses RNA to replicate. Without DNA’s built-in “proof-reading” capabilities, RNA viruses like influenza and HIV are more prone to genetic errors during replication, allowing them to mutate quickly as they move from host cell to cell. In the case of influenza, the virus is continually finding new ways of changing the surface proteins that help it attach to a host cell, effectively staying one step ahead of our immune systems.
The seasonal flu vaccine was invented by biologists Jonas Salk and Thomas Francis for the US military, just prior to the outbreak of the Second World War. Updating the vaccine is now the work of highly skilled microbiologists, epidemiologists, physicians, and other public health experts who, every season, try to match the components of the flu vaccine with the circulating strain of virus. Unfortunately, some active strains of influenza mutate to the point that the vaccine’s potency is diminished. According to the CDC, “It is not possible to predict how well the vaccine and circulating strains will be matched in advance of the influenza season, nor is it possible to predict how this match may affect vaccine effectiveness.”
Despite this, flu shots shots tend to provide modest to high protection against the flu each year, decreasing the number of missed days of work by a half day on average.
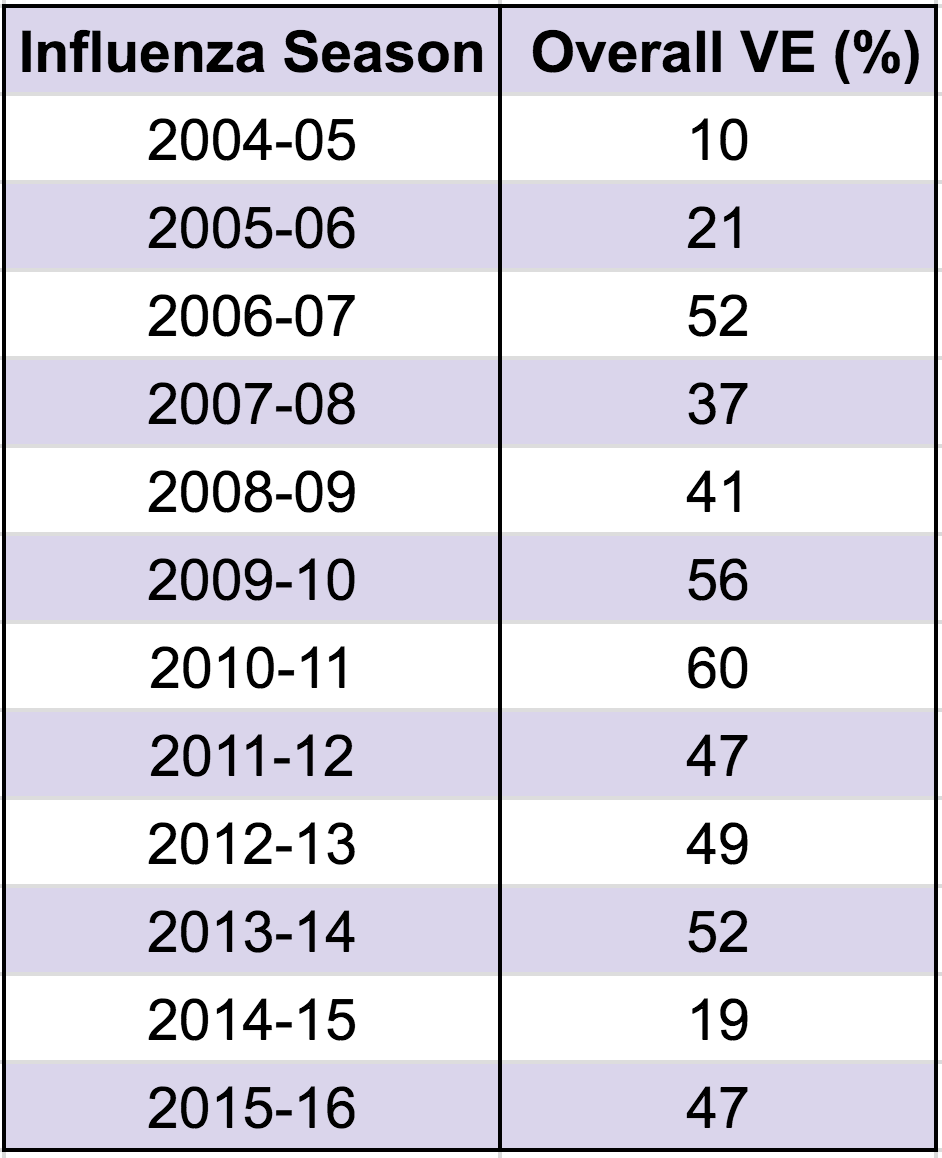
Vaccine effectiveness (VE) for influenza seasons 2005-2016. (Source: CDC)
Compared to previous years, the 2016-17 flu shot is about as good as can be expected, if not better. Looking at the effectiveness of vaccines since 2004-05, it’s clear that flu shots tend to be all over the map in terms of performance. The most effective shot appeared during the 2010-11 season, conferring 60 per cent protection, while the disastrous shot of 2014-15 was only 19 per cent effective. Since 2004-05, the average effectiveness has been 40 per cent, jumping to 42 per cent over the past five years.
The dramatic ineffectiveness of the 2014-15 shot is a regrettable dip in the data, but it’s to be expected given the nature of the ever-drifting flu. That season, two-thirds — and possibly as much as 80 per cent — of circulating H3N2 viruses had mutated from the vaccine. The following year, the flu shot rebounded.
For the most part, the flu shot does its job. For the past seven years, the CDC has published its annual estimates on the number of illnesses, medical visits, and hospitalizations prevented by vaccinations each year. During the 2012-13 flu season, for example, when the shot was 49 per cent effective (just like this year), it prevented 5.6 million flu illnesses, 2.7 million flu-related medical visits, and about 61,500 flu-related hospitalizations.
Despite the relatively effectiveness of this year’s shot, the 2016-17 flu season has been a nasty one. The season has been dominated by the influenza A H3N2 viruses, and cases have been spiking across the US over the past eight weeks. Regions in the US northwest had it bad early, but these states are now on a downswing. The midwest and the East Coast are now experiencing a jump in flu activity, particularly the rate of infections for the influenza B viruses, which tend to make the rounds later in the season.
[referenced url=”https://gizmodo.com.au/2015/09/the-flu-vaccine-that-lasts-a-lifetime-is-coming/” thumb=”https://i.kinja-img.com/gawker-media/image/upload/t_ku-large/1401642549006528580.jpg” title=”The Flu Vaccine That Lasts A Lifetime Is Coming” excerpt=”The flu vaccine. a tedious annual chore, but necessary unless you want to spend a week bed-ridden and barfy. Still, wouldn’t it be great if one jab could protect you for life? A lifetime flu vaccine isn’t impossible, and we’re making progress toward one, but we’ve still got a ways to go.”]
Looking to the future, it’s wholly possible that a universal flu vaccine will be developed — that is, a vaccine offering lifelong protection. Currently, teams in Canada, the US, and the UK are working on the problem, but given what we know about the virus and its penchant for mutation, it’s not going to be easy. The key to developing a universal vaccine is to find aspects of the virus that are (1) consistent across all strains and (2) aren’t susceptible to change. One possibility, as noted by Richard Antrobus of Nuffield’s Department of Medicine in the UK, is to use the body’s immune system to target and disable key internal proteins within the flu virus.
Antrobus says a universal vaccine could eventually replace the normal seasonal flu jab. “That is certainly the ultimate goal, but that is going to be particularly challenging,” he noted in a NDM release. “Our vaccine candidate is designed to protect against different strains within Influenza A, but there is also an Influenza B. So a truly universal vaccine will need to cross both of those strains, which will be quite difficult.”
In other words it could be years, possibly decades, before we see that universal shot. In the meantime, if you didn’t get your flu shot this year, just remember that it’s not too late.
