Being diagnosed with cancer is often compared to being kicked in the gut — by a Clydesdale. But if caught soon enough, many of the disease’s 200 iterations offer more than even survival rates, five years down the line. It’s by no means a clean bill of health, mind you, but there several forms of cancer that modern science has beaten back.
Now, don’t get me wrong, no cancer diagnosis is a laughing matter. We’re in no way advocating any form of alternative treatment or publishing this to provide any sort of medical advice. Quite honestly, if you’re getting your medical advice from the internet, please bludgeon yourself with a tack hammer and be sure to ask the attending physician what’s on your mind while getting patched up in the ER.
That being said, it’s worth taking a look at the statistics of diagnosis to see what’s being done right, and where we still have a ways to go.
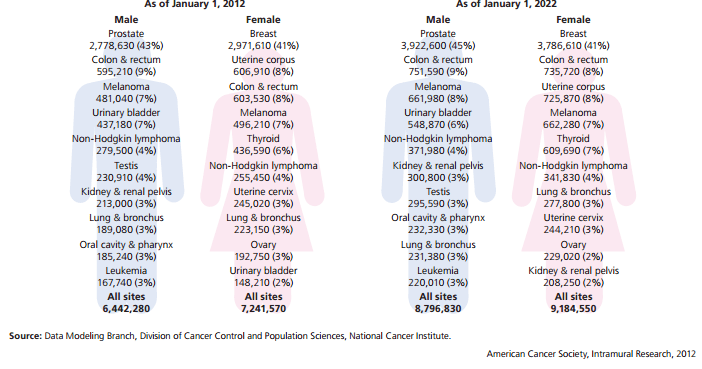
The prevalence of various cancers in 2012 and estimated for 2022.
Breast Cancer
Breast cancer is the single most common form of cancer in women, accounting for nearly half of all diagnoses. On average 1 in 8 Australian women will suffer from breast cancer in her lifetime. However, with early discovery and treatment, you’ve still got a better than 90 per cent chance of surviving for the next five years at least.
The two most common forms of breast cancer are known as Ductal carcinoma, which affects the ducts that transport milk from the inner breast into the nipple, and Lobular carcinoma, which afflicts the milk gland themselves. Both forms start as non-invasive, though not benign, growths (called “in situ”) but if left untreated can quickly invade other organs.
Like many cancers, we only have a rough idea of what could potentially cause it, though we do know that the common risk factors — specifically age, genetic factors, personal health history, and diet — all play a role in one’s breast cancer risk.
Exams
You’ve found a lump. Don’t freak out, just make an appointment with your doctor as soon as possible. Your physician, as part of the exam, should both quiz you about your personal and family health history and perform a physical exam of your upper torso including both breasts, armpits, neck and chest.
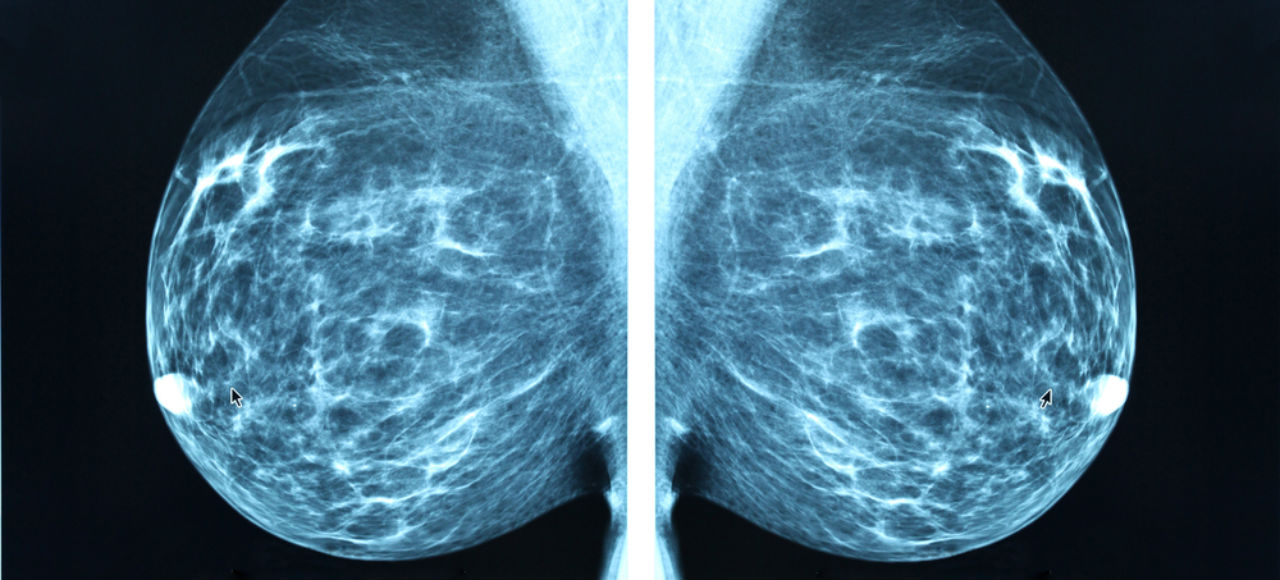
Depending on what she finds, your doctor could order additional tests including a mammogram, MRI,or CT scan to get a clearer image of the lump, an ultrasound to determine whether the lump is solid or fluid-filled, or directly biopsy the mass for testing. The doctor may also recommend a PET (positron emission tomography) scan or Sentinel lymph node biopsy to ensure that, if it is cancer, it hasn’t become invasive (which is bad) or spread to the lymph system (which is very bad).
Treatment
Once your doctor has a handle on the state of your condition (known as “staging”) treatment can begin. The steps your doctor takes depend on type and stage of the cancer, and whether the cancerous cells overproduce a gene called HER2/neu (which is sensitive to estrogen and reproduces out of control in its presence).
Common treatments include the standard “Scorched Earth” measures of radiation and chemotherapy. Chemotherapy drugs can be administered either orally or intravenously and are designed to kill cancer cells, halt their spread and ease their symptoms. Radiation therapy on the other hand exploits two phenomena — a) that cancer cells grow and reproduce far faster than regular cells and b) radiation kills rapidly growing cells more often than regularly growing cells — to generally target, kill and contain malignant tumours. Because chemotherapy affect the patient’s entire body, it’s known as a systemic treatment. Radiation therapy, conversely, is considered a local treatment as it only affects a small portion of the body. Surgery, either a lumpectomy to remove just the offending mass or a mastectomy to remove the entire breast, may be necessary as well.
A newer treatment involves hormone therapy. If the cancer overexpresses the HER2/neu gene, it will grow and divide out of control in the presence of estrogen. Hormone therapies such as tamoxifen or a separate class known as aromatase inhibitors block the effects of estrogen (or halt its production entirely), starving the tumour of the chemical it needs to thrive and have been shown to be very effective at helping postmenopausal women.
Depending on the stage, location and type of cancer your doctor finds, you may undergo a combination of one or more treatments. [Cancer Australia]
Picture: Blue Planet Earth
Cervical Cancer

While not as prevalent as breast cancer, cervical cancer does carry a higher five-year mortality rate of 28 per cent. Beyond the conventional risk factors discussed above, research has shown a strong link between contracting human papillomaviruses and cervical cancer in women.
In fact, according to the Cancer Council, four out of five people have at least one type of HPV at some point in their lives. HPV is divided into low risk variants such as types 6 and 11, which are responsible for almost all cases of genital warts, and a dozen or so high-risk variants such as types 16 and 18, which have been shown to cause a majority of HPV-related cancers.
While most cases of HPV clear up on their own thanks to your own natural defences, stubborn HPV variants that linger within the body have shown a high propensity to instigate cancer. That’s why it’s absolutely essential for women to take two proactive steps to protect themselves: get regular cervical cancer screenings throughout their lives and receive an HPV immunisation before they become sexually active. Note that these aren’t mutually exclusive — even if you do receive an immunisation, it only lowers your chances of developing cancer, not eliminate it, so you must still get routine cervical exams.
Exams
If you notice symptoms of cervical cancer — such as off-cycle menstrual bleeding or pain during sex, your doctor will perform a number of physical exams including, but not limited to, a Pap smear, a visual inspection of the cervix using a colposcope or a biopsy of suspect tissues.
Treatments
Depending on the size and stage of the cancer — stage 0 denotes that the cancer is still confined to the cervix itself and has not spread, while stage IV denotes that it has fully metastasized and spread to other organs in the body — your doctor will prescribe a combination of treatments. As with breast cancer, you may be asked to undergo chemotherapy, radiation therapy or surgery to remove the offending growth. Your desire to become pregnant one day will also play an important role in determining your course of treatment. [Cancer Council]
Picture: Artem Furman
Skin Cancer
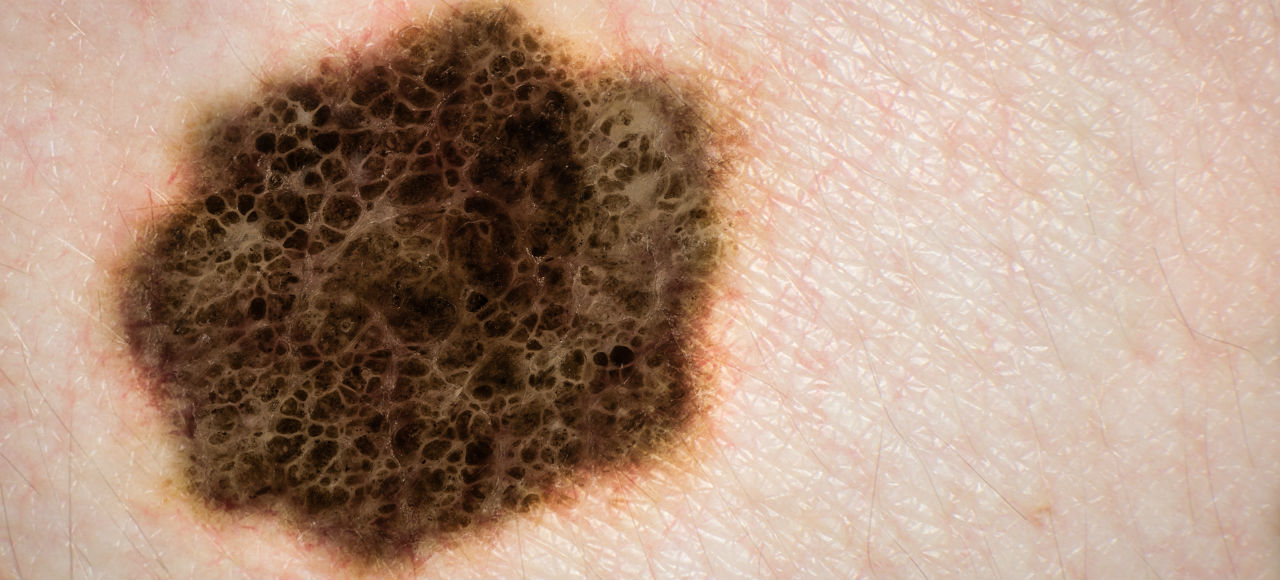
Depending on the form that you contract, skin cancer can be little more than a minor inconvenience. For the estimated 400,000+ diagnoses of nonmelanoma cancer in Australia each year, less than 500 are expected to be at risk of dying from it. That said, for the estimated 12,500 people diagnosed with the serious form of skin cancer, melanoma, it can be quite deadly.
The lesser types of skin cancer, specifically the basal and squamous cell varieties, are found at on the outermost layers of your skin and are typically triggered by excessive sun exposure in addition to the normal variables of age, sex, family history and so forth. While these cancers can grow quickly, they typically remain in situ and spread slowly. If discovered and treated early enough, your chances of surviving are damn well near 100 per cent.
Melanoma, not so much. As the Cancer Council explains:
An individual’s prognosis depends on the type and stage of cancer, as well as their age and general health at the time of diagnosis. Five year survival for people diagnosed with melanoma is 91%, rising to 99% if the melanoma is detected before it has spread. If spread is within the region of the primary melanoma, the five year survival is 65%, dropping to 15% if the disease is widespread.
So if you don’t want your largest organ turning against you, be sure to slather on the sunscreen, limit your exposure to natural and artificial UV sources, and immediately report any weird new moles you find to your doctor.
Exams
In addition to interviewing you and physically examining the growth, biopsies are the method of choice when identifying skin cancer. Your doctor may opt for a shave or punch biopsy, where a scalpel or punch tool is used to cut off or gouge out a small portion of the growth. Your doctor may go for an incisional biopsy, where the entire growth is sliced out, or an excisional biopsy may be required in the case of suspected melanomas. That involves cutting out not just the growth but a small amount of surrounding tissue. See, melanoma has a nasty habit of spreading to the lymph system, so cutting out additional flesh can help prevent its spread. Your doctor may also refer you to a dermatologist for further tests including dermatoscopy (aka epiluminescence microscopy) to get a better look at your skin.
Treatments
For non-melanomas, treatment is straightforward: cut that sucker out. The doctor may employ a technique known as Mohs micrographic surgery, which involves setting up a microscope just above the growth then using that to visually check for the presence of cancer cells as the doctor shaves off layers of your skin like prosciutto until no more cancer cells remain. Cryosurgery, which freezes the growth off like a wart, can also be used.
For melanoma, the treatment will depend on the size, location and stage of the cancer. For early stages, a simple excision may be all that’s needed. For more advanced stages, especially if the cancer has spread to your lymph system, more aggressive surgery as well as an immunotherapy regimen of interferon or interleukin-2, immunotherapy chemotherapy and radiation therapy may be required. [Cancer Council – Melanoma Institute Australia]
Picture: Australis Photography/Shutterstock
Prostate Cancer
Even though you have, on average, a 92 per cent chance of surviving prostate cancer, it is not something to be lax about. Unlike other forms of cancers, prostate cancer has a number of clear risk factors including age (it’s common among retirees but exceedingly rare among people under 40), race and sex (men of African descent are at a higher risk developing prostate cancer at any age), family history and occupation. Men who have been exposed to Agent Orange, who farm, paint, work in tyre plants or have handled cadmium regularly over their lives are also much more likely to develop prostate cancer.
Exams
Bend over and try to relax; the only way your doctor will be able to tell if you’re developing prostate cancer is through a digital rectal exam. If your doctor notices something wrong, a prostate biopsy as well as a prostate-specific antigen (PSA) blood test may be recommended.
The PSA test measures the amount of these specific antigens in your blood. A normal PSA level is considered to be 4.0 ng/ml (nanograms per millilitre of blood), although for guys under 50 that number is around 2.5 and slightly above that for older guys. Increased levels of PSA indicate a heightened risk of developing prostate cancer but cannot diagnose that you actually have it — only a biopsy can do that.
The results of your biopsy are calculated into what’s known as a Gleason Score. As the NIH explains:
The biopsy result is reported using what is called a Gleason grade and a Gleason score. The Gleason grade tells you how fast the cancer might spread. It grades tumours on a scale of 1 through 5. You may have different grades of cancer in one biopsy sample. The two most common grades are added together. This gives you the Gleason score. The higher your Gleason score, the more likely the cancer can spread beyond the prostate:
- Scores 2 through 5: Low-grade prostate cancer.
- Scores 6 through 7: Intermediate- (or in the middle) grade cancer. Most prostate cancers fall into this group.
- Scores 8 through 10: High-grade cancer.
If you score a 6 or higher, you doctor may also recommend CT or bone scans, or an MRI, to ensure that the cancer has not spread to other organs.
Treatments
Since some iterations of prostate cancer are hormonally charged, like the estrogen-loving HER2/neu breast cancer variant, your doctor might prescribe testosterone-blocking hormonal treatments (especially if it’s already spread). Otherwise the normal mix of radiation therapy, chemotherapy, immunotherapy and varying degrees of surgery will be employed to ridding you of your malfunctioning cells. [Prostate Cancer Foundation of Australia]
Picture: Juan Gaertner
Testicular Cancer

Thankfully, testicular cancer in Australia is both relatively rare and quite survivable. It accounts for 1.2 per cent of all new cancers in men and has a survival rate of around 98 per cent. It’s the second most common form of cancer for men between the ages 18 to 39, and it afflicts white guys far more than African and Asian males. But unlike prostate cancer, we really don’t know what incites the development of testicular cancer. There’s suspicion that chemical and viral exposure may play a part, but no definitive proof either way has been uncovered to date.
This cancer comes in two basic flavours: the slow-growing Seminoma that usually manifests in the 30s and 40s, and the fast-growing Nonseminoma that affects multiple cell types within the testicle.
Exam
You’ve found a lump. Don’t freak out, just make an appointment with your doctor as soon as possible. Your doctor, as part of the exam, should both quiz you about your personal and family health history and perform a physical exam of your ball sack. You doctor might begin by holding up a light to your scrotum (to see if light penetrates the lump) before ordering more tests. These may include an abdominal and pelvic exam, various antigen-based blood tests, x-rays and scrotal ultrasounds.
Fortunately, because you have two of them, one of your balls is superfluous to necessity. Just as with diagnosing a rabid dog, the only way to see if your testicle is really infected with cancer is to kill it and cut it open — or, rather, surgically remove it and biopsy the mass. Only then will the doctor be able to definitively tell the tumour type and stage — hopefully, the cancer has not yet spread into the rest of your pelvis, bladder or lymph system.
Treatment
Since one of your family jewels has already been mined, you’re SOL on that little guy. Thankfully, seminomas are really weak against radiation, so while you may have to irradiate your baby maker, you won’t have to do it much. If the cancer has spread, a systemic round of chemotherapy may be prescribed — and has proven super-effective against both forms of testicular cancer.
Overall, if you catch a seminoma in its first stage, before the cancer spreads to the lymph nodes, you have a 95 per cent survival rate. Even with stage II and III, your chances of dying are just slightly higher. [Cancer Council]
Picture: elnavegante/Shutterstock
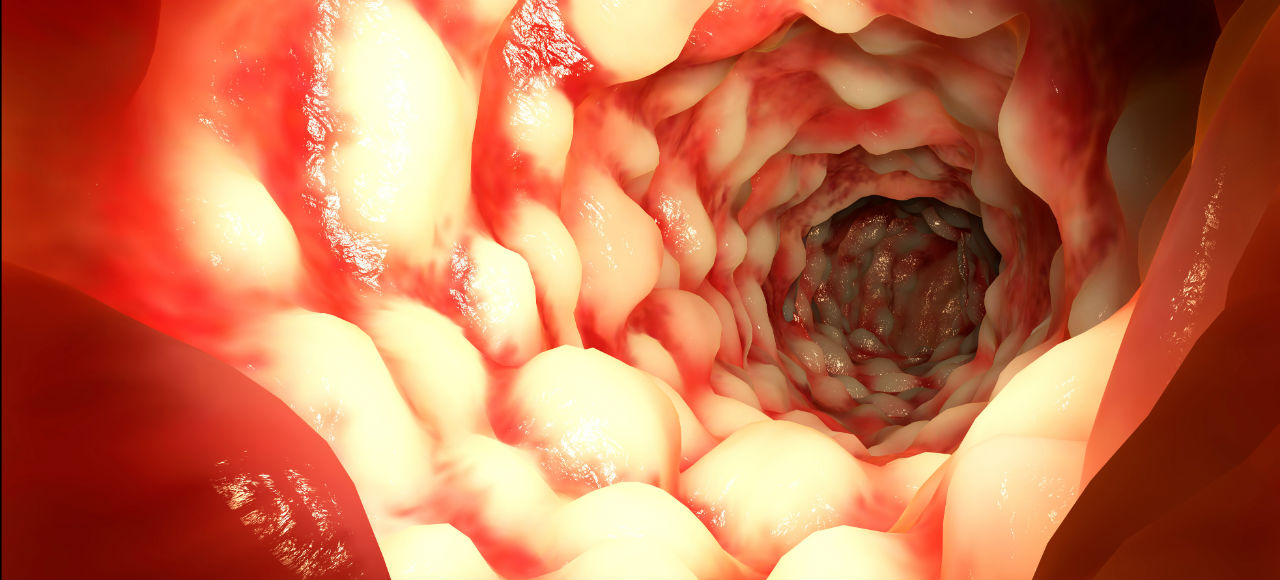
Bowel Cancer
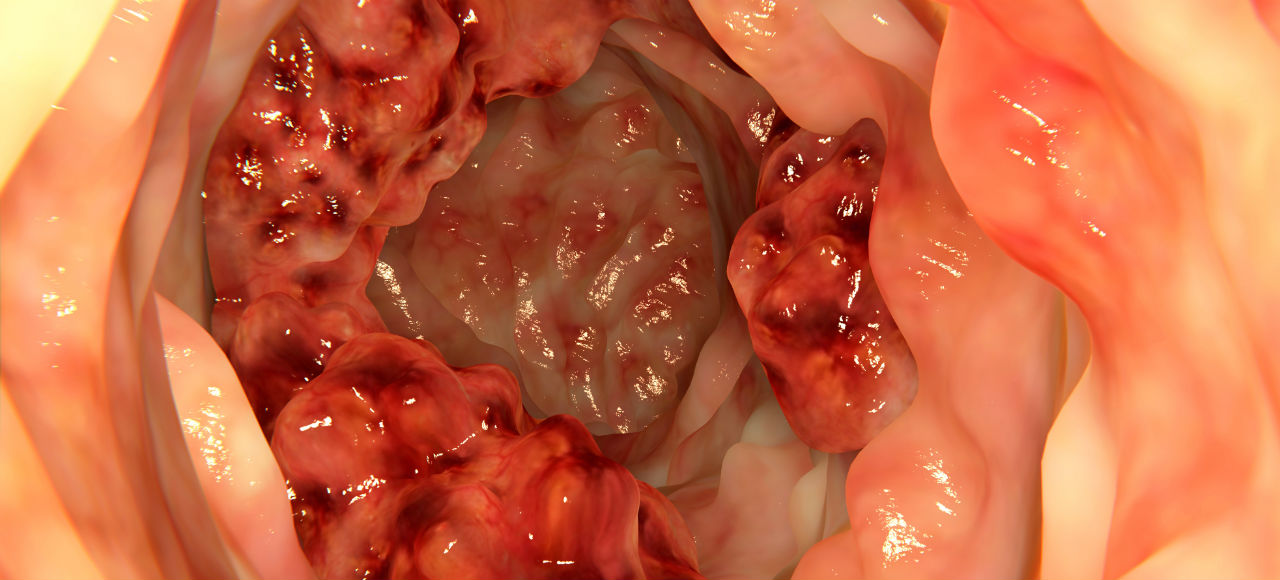
Bowel cancer is among the leading causes of cancer-related deaths in Australia, although with prompt treatment it can often be completely cured. This cancer affects the glands that inhabit the lining of your colon running from the small intestines to the rectum. Oddly, most forms of bowel cancer begin as benign polyps in these glands that only gradually turn cancerous.
As with the other cancers, we don’t know what triggers it for sure, but certain risk factors will increase your chances of developing it. These include being over 60, being of African or Eastern European descent, and having a family history of the disease. There is also a growing amount of evidence that this cancer may be linked to high-fat, low-fibre diets, as well as your smoking and drinking habits.
Exam
As with the other testing procedures, bowel diagnoses begin with a physical exam of the abdomen and/or rectum (depending on if your doctor suspects colon or rectal cancer). A faecal occult blood test may also be administered — don’t worry, the only black magic involved is looking for blood in your poop — as well as a colonoscopy.
Treatments
Unfortunately, your treatment options for bowel cancer are pretty much limited to chemotherapy, radiation therapy and surgery. For the first three stages of bowel cancer, the preferred method is known as colon resection, wherein the offending length of colon is simply cut out. [Cancer Council]
Picture: Juan Gaertner/Shutterstock
Unfortunately, not all forms of cancer are as easily diagnosed and treated as those discussed above. Three types are especially virulent in their ability to avoid detection, rapidly spread and kill you within five years: lung, liver and pancreatic cancer all offer little hope, with five-year mortality rates topping 85.9 per cent, 84.5 per cent and 94.8 per cent, respectively. It’s not uncommon for pancreatic and lung cancer patients to be diagnosed after they have already reached the terminal stage of their disease and have days, maybe weeks, to live.
Still, it’s encouraging to know that while we haven’t beaten cancer yet, we’ve taken it head on in many of its forms and often come out on top. Hopefully, someday soon, this list will be a whole lot longer.
Lead picture: jovan vitanovski